GYNAECOLOGY DEPARTMENT
The best for you.
Contact
Contact
Gavra Vukovića b.b, Podgorica
Dentistry: 020 227 227
Polyclinic: 020 227 224
Gynecology: 020 227 444
Department is open on all days except Sunday. Our nurses will answer all your questions regarding appointment and doctor availability, consultation scheduling, treatment prices and provide all other relevant information, in person or via phone call.
Specialized hospital Ars Medica cooperates with the Healthcare Fund of Montenegro. Insured patients have the right for three free-of-charge IVF attempts.
Department of Gynaecology and the IVF Centre of Specialized hospital Ars Medica are the first medical departments in Montenegro in compliance with ISO healthcare and management standards.
GYNAECOLOGIC EXAMINATION
Care in the first place.
Gynaecologic examination consists of preliminary analysis or control check-up, and may employ various diagnostic tests such as Papanicolaou test, bacteriologic, virologic and fungal analysis.
PAPANICOLAOU TEST
This test is short and easy to preform.
Colposcopy
Colposcopy is a procedure of examining cervix and vagina, diagnostically aimed at identifying distribution of abnormal squamous cell epithelium and screening for early signs of cervical cancer.
GYNAECOLOGIC PROCEDURES AND OPERATIONS IN GENERAL AND LOCAL ANESTHESIA
Pregnancy termination can also be medically indicated. The procedure can be preformed in both local and general anaesthesia. Preparation consists of ultrasound examination and laboratory analysis.
Explorative curettage is an intervention preformed in case of prolonged bleeding, postmenopausal bleeding, or for other unclear situations that necessitate sampling the tissues of endocervix or endometrium for the purpose of definitive diagnosis.
Cervix biopsy is an intervention that consists of taking a sample from suspicious location discovered during the colposcopy of cervix.
Cervical conisation is an intervention of excision of a cone shaped tissue from the cervical mucus membrane, in cases of premalignant epithelial lesions of cervix.
LOOP procedure is a minimally invasive excision method for atypical cervical transformations.
Condyloma removal is a procedure with a high success rate, that can be preformed using multiple minimally invasive methods such as laser removak,cryotherapy, electrocoagulation, etc. However, it is impossible to totally remove HPV virus from the organism.
ULTRASOUND EXAMINATION
Details.
High resolution real time imaging enable us to examine fetus in real time, and assess various aspects of growth and development.
The possibility of monitoring the development, biometrics and assessment of fetus and circulation, make ultrasound an indispensable tool for maintaining healthy pregnancy.
ULTRASOUND EXAMINATION IS USED FOR:
ULTRASOUND IS INDISPENSABLE IN PATHOLOGIC DIAGNOSTICS OF:
Ultrasound
PREGNANCY COUNSELLING
Step by step…
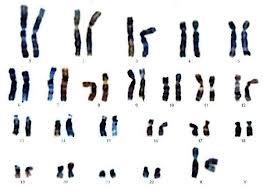
NIFTY- NON-INVASIVE PRENATAL TEST FOR DIAGNOSIS OF CHROMOSOMAL TRISOMY
“Low risk” test result indicates near certainty of healthy pregnancy. “High risk” test result indicates high chance of trisomy existence. In a case of “high risk” result, it is advised to proceed to more detailed diagnostic testing.
Discovering of chromosomal abnormality during pregnancy is done through combination of screening and diagnostic tests. If the tests indicate high risk, doctor will recommend amniocentesis.
Chromosomal trisomy is reported as present in only 3% of cases. Problem is posed by an increasing number of pregnant women carrying healthy fetus that are unnecessarily directed to the further invasive diagnostic screenings which carry a risk of miscarriage (0.8%-2% of cases) .
This test is available for single and twin pregnancies. Test cannot diagnose genetic mutations, chromosomal mosaicism or structural chromosomal abnormalities.
Although the testing is possible from 10th week of pregnancy, it is recommended to obtain blood sample from 12th -24th weeks of pregnancy.
Analysis of sex chromosomes will indicate the gender, unless it is a case of twin pregnancy.
Test reliability may be influenced by following factors: transfusion, transplantation, immuno-therapy or stem cell therapy, presence of mosaicism in fetus, placenta, or mother.
Test is not recommended in case of twin pregnancy characterised by disappearance of fetus (vanishing twin) .
Test results are known after 10-14 days.
Prior to testing, it is recommended to consult your gynaecologist.
NON-INVASIVE PRENATAL DIAGNOSTICS

Double test AFP + hCG
Triple test AFP,E3,hCG
Quadruple test AFP,hCG,E3 + inhibinA
INVASIVE PRENATAL DIAGNOSTICS
Chorion biopsy CVC
Choriocentesis is prenatal diagnostic method used to extract chorion sample for examining genetic structure of an embryo.
Method is used in patients older than 35, or with higher risk of genetic disease.
The procedure is preformed between 8th and 12th week of pregnancy
Amniocentesis
Amniocentesis is a prenatal diagnostic method used for examining genetic structure of the fetus through amniotic fluid analysis. This method is used in case of high risk of genetic diseases.
The procedure is preformed between 15th and 20th week of gestation. Testing results are available in 15 days.
Cordocentesis
Cordocentesis is umbilical sampling of fetal blood. It is preformed In local anaesthesia with complementary ultrasound monitoring.
Cordocentesis can be preformed multiple times throughout the course of pregnancy.
It can diagnose hereditary and intrauterine disorders, and is used for assessment of the state of fetus in last trimester of pathologic pregnancies.
The procedure can be preformed from 22nd week of gestation to labour.
CONTRACEPTION
Be sure
Intrauterine metallic supplement (IUU)
For patients using anticonvulsive medication
For diabetes mellitus patients
For patients with benign or malignant breast neoplasm
For hypertensive patients
For patients that experienced ceretrovascular insult (cannot use hormonal contraception)
Intrauterine supplement with hormone addition IUS
For patients with menstrual frequency and intensity disorders.
For endometriosis and adenomiosis patients.
Oral contraception

Oestrogen-progesterone tablets are usually taken 21 days + 7 day break characterized by abrupt haemorrhage similar to menstrual bleeding. Progesterone pills are taken continuously without the brake.
Oestrogen-progesterone tablets are more popular because they maintain stabile cycles. Progesterone pills are characterized by irregular haemorrhages or absence of menstruation. They are frequently used for post—labour protection, during the breastfeeding.
Adverse effects:
Contraception pills can cause temporary sickness, headache and chest tension. These symptoms usually subside quickly.
During the first cycles, it is possible to experience some irregularity in bleeding pattern, outside the expected time frame. This can occur as a result of your body getting used to the contraceptive, or due to the simultaneous medication taking (antibiotic, antiepileptic), or designating very low hormone doses.

Other adverse effects include decreased libido, depression, weight gain, affected carbohydrate, protein and fat metabolism, affected coagulation factors with increased risk for thrombosis and embolism (particularly after the age of 35) In smokers.
Contraindications:
Contraceptive pills are absolutely contraindicated in patients suffering from acute or chronic liver and gallbladder diseases, presence of thrombosis or embolism in anamnesis, presence of antiphospholipid antibodies, hypertension, diabetes mellitus, breast cancer, undiagnosed vaginal haemorrhage.
Relative contraindications are: mild hypertension, diabetes, liver disease, angina pectoris, smoking, breastfeeding, mastopathy , myomas, cardiac surgeries, renal insufficiency, etc.
Further screening and analytics are preformed at the clinic after the initial specialist examination.



